The Crisis Roadmap
Crisis Continuum
Values-Based System and Program Design
Measurable Criteria for an Ideal System
Services Address The Continuum of the Crisis Experience
Creating Safe Spaces That Are Warm, Welcoming and Therapeutic
Measurable Criteria for an Ideal Crisis Space
Safety and Security Practices That are Both Safe and Welcoming
Measurable Criteria for Safety and Security Practices That are Both Safe and Welcoming in an Idea System
Treat Law Enforcement as a Preferred Customer
Measurable Criteria for an Idea Crisis Continuum That Treats Law Enforcement as a Preferred Customer
Crisis Center of Crisis Hub
Call Centers and Crisis Lines
Deployed Crisis-trained Police and First Responders
Medical Triage and Screening
Mobile Crisis
Behavioral Health Urgent Care
Intensive Community-based Continuing Crisis Intervention
23-hour Evaluation and Extended Observation
Residential Crisis Program Continuum
Role of Hospitals in Crisis Services
Transportation and Transport
 DEPLOYED CRISIS-TRAINED POLICE AND FIRST RESPONDERS
DEPLOYED CRISIS-TRAINED POLICE AND FIRST RESPONDERS
In the United States, the primary responder to a mental health crisis is often a law enforcement officer. In Florida, law enforcement officers initiate more involuntary commitments annually than the total combined number of arrests they make for robbery, burglary and grand theft auto. Other first responders that may be under the auspice of the fire department or independent providers, notably the EMS systems, are often on the scene as part of behavioral health crisis response as well. Although one goal of the ideal crisis system is to shift the bulk of crisis “first response” to behavioral health clinical crisis settings, law enforcement and other first responders will still be initial or early contact in many crisis situations. In some systems, emergency medical technicians (EMTs) have been trained to provide mobile crisis services and/or to provide continuing crisis visits to high utilizers.
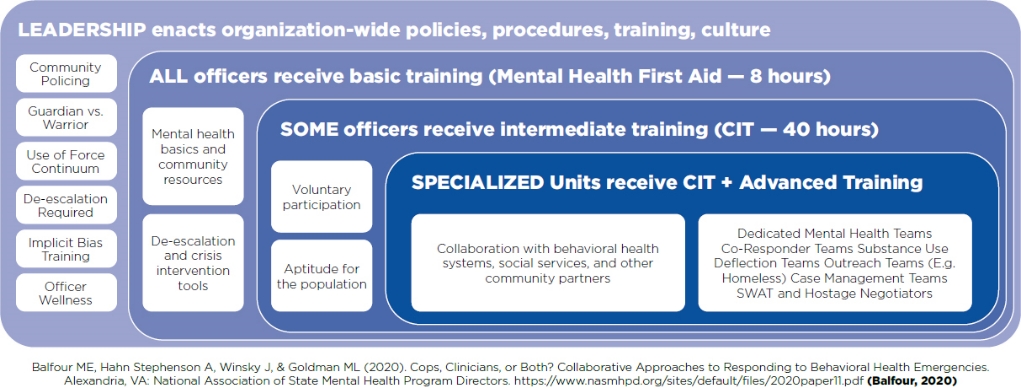
As long as law enforcement officers and other first responders are part of the team of primary responders to behavioral health crises, it is critical that they are appropriately trained to use best practices in a coordinated and collaborative fashion with other crisis providers and community stakeholders. There are standard training packages that all first responders should be introduced to and selected first responders should receive in full and be deployed to be available preferentially for crisis response – CIT training is a notable example. In addition, there are identified standards for how police and first responder training and deployment should occur as part of community crisis planning. These standards should be followed in an ideal crisis system.
Measurable Criteria For An Ideal System
The accountable entity works with the community collaborative, especially first responders (e.g., law enforcement agencies, EMS) to develop and implement a plan for first responder training and deployment, as follows:
Collaborative planning and implementation
Police and first responder success and effectiveness in responding to a mental health emergency depend on the commitment of stakeholders throughout the community. Cross-system collaboration is essential for the transition from the criminal justice system to the community mental health system. Program operations must rely on collaboration among community stakeholders including: the State Attorney’s/District Attorney’s Office, the Public Defender’s Office, the County Department of Corrections and Rehabilitation, the States’ Department of Children and Families, the local behavioral health authority, the Social Security Administration, public and private community mental health providers, law enforcement agencies, local school systems, colleges and universities, emergency medical technicians, family members and mental health consumers.
Bureau of Justice Assistance (BJA) 10 Steps
BJA developed a Police Mental Health Collaborative guidance document and identified 10 essential elements necessary for an effective law enforcement response to people with mental illnesses:
- Collaborative planning and implementation.
- Program design.
- Specialized training.
- Call-taker and dispatcher protocols.
- Stabilization observation and disposition.
- Transportation and custodial transfer.
- Information exchange and confidentiality.
- Treatment supports and services.
- Organizational support.
- Program evaluation and sustainability.
Deployment of adequate numbers of CIT trained officers
Communities should adopt the CIT training model developed in Memphis, Tennessee. Known as the Memphis Model, the purpose of CIT training is to set a standard of excellence for law enforcement officers with respect to treatment of individuals with mental illnesses. All officers should have basic exposure to an introductory curriculum on behavioral health such as MHFA for Public Safety. CIT officers receive more intensive training, including 40 hours of specialized training in: psychiatric diagnoses, suicide intervention, substance use disorders, behavioral de-escalation techniques, trauma, the role of the family in the care of a person with mental illness, mental health and substance use disorder laws and local resources for those in crisis.
CIT officers perform regular duty assignment as patrol officers but are also available and deployed to respond to calls involving mental health crises. In many systems, CIT officers are deployed with mobile crisis workers in coresponder teams. In other systems, the CIT officers and mobile crisis collaborate but work independently. In either case, CIT officers must be skilled at de-escalating crises involving people with mental illnesses while bringing an element of understanding and compassion to these difficult situations. When appropriate, individuals in crisis should be transported to a crisis center in lieu of being arrested and taken to jail.
Law Enforcement: Organizational approach to serving community members with behavioral health needs
CIT homeless resource officers (HROs)
This new type of unit focuses on the most chronically ill homeless population with a history of mental health and substance use. The HRO identifies individuals meeting criteria for this unit. A case file includes a photo of the client, criminal history printout, mental health and substance userelated arrests and court/provider related documents. If the individual meets criteria, the HRO:
- Files a Petition for Involuntary Treatment with courts and attends court proceedings.
- Contacts the behavioral health entity in reference to a treatment bed.
- Continues engagement until a treatment bed becomes available.
- Transports client to treatment facility.
- Participates in weekly follow-ups/case staffing on clients’ progress.
- Informs area officers of the clients transitioning into treatment.
- Attends monthly meetings at police headquarters with behavioral health entity, area police commanders/city’s Homeless Outreach Team.
- Follows client until graduation.
CIT coordinator
A CIT coordinator should be selected outside the local law enforcement department and assigned to the local accountable behavioral health entity or crisis hub provider. The coordinator should be responsible for planning, coordinating and implementing all CIT-related classes, including the 40-hour CIT class, roll call training, recurring training, 911 call-taker training and executive training for the chief/sheriff and their majors. The CIT coordinator should also be trained and prepared to field referrals from law enforcement officers for their own personal mental health treatment needs.
CIT liaisons
CIT liaisons from each department and police station should be selected to meet quarterly with the CIT coordinator and behavioral health providers to share information about situations and cases that need further coordination and intervention. CIT liaison officers should attend all community behavioral health/criminal justice coordinating meetings. When practical, the community should recognize and award CIT Officers of the Year.
Avoidance of law enforcement transport
When appropriate, behavioral health professionals should become the first responders to mental health emergencies and CIT-trained law enforcement officers should serve as backup, if needed. When appropriate, transportation for an involuntary examination should be by a behavioral health professional in a civilian vehicle or ambulance, not in a marked police vehicle.
Jail diversion continuum
CIT should be part of a larger coordinated community diversion program to keep individuals with serious mental illnesses out of the criminal justice system when appropriate and in the behavioral health treatment system. Description of all elements of a continuum of jail diversion services in accordance with the sequential intercept model is beyond the scope of this report.
IN THE STORY OF MR. Y:
A crisis call center would certainly have dispatched more appropriate first responders to Mr. Y and avoided his arrest and transportation by police to a law enforcement facility.
